It is common to have problems going to the toilet after critical illness and this includes problems with having a poo. If this happens often, you could have constipation. Signs of constipation include:
- having a poo less than three times a week
- difficulty and pain when having a poo
- having to strain a lot when having a poo
- poo that is like small hard pellets
- feeling that you haven’t been able to get all the poo out.
What can cause constipation?
To understand what causes constipation, it is helpful to know how poo is made. The food which you eat is broken down in your stomach. Any liquid and food moves from the stomach into the first part of your digestive tract (called the small bowel) which is where nutrients and energy is taken up by the gut lining. This leaves some food that can’t be used by your body and it goes into your large bowel. This is mixed with fluid in your body and forms poo. To help the poo come out of your body, your large bowel has muscles which tense up and relax to push it towards your rectum (bottom) until you have the feeling that you need to go to the toilet.
Constipation can happen after critical illness because of all the medications you had or because of the stress your body has been through.
You might also get constipation if:
- there is not enough water in your poo, which makes it very hard to push out
- muscle contractions in the large bowel are too slow or weak, which means the poo doesn’t move through your body quickly. This means poo can stay in the same place for hours or days and make it drier and harder.
The good news is that there are many things that can help constipation, including exercise and what you eat and drink.
What can I eat to help constipation?
The main type of food to help constipation are those that are high in fibre. Fibre is the part of plant foods that cannot be absorbed into the gut lining and so it provides bulk to poo. It can help constipation by making each poo bigger but also by acting like a sponge, absorbing water into the poo, which makes it softer and move through your body more easily.
Many of us don’t eat enough fibre, so it is important to increase fibre intake slowly while your body gets used to it. It also helps to drink enough when having more fibre. This also helps food to go through your body and helps the poo to be softer. Try and drink a glass of water with every meal.
There are two types of fibre which can help constipation:
Insoluble fibre which helps to provide bulk to the stool and is often called ‘roughage’. It is found in foods such as wheat bran, vegetables and whole grains.
Soluble fibre dissolves in water and helps slow down how the food goes through our body, which means it gives us energy for longer. This fibre is found in:
- oats, barley or rye
- fruits such as apples, pears, blueberries and citrus fruit
- vegetables such as broccoli, cauliflower, cabbage, sweet potatoes, avocado and onions
- seeds and nuts, such as pumpkin and sunflower seeds and most nuts
- flaxseed, linseed and chia seeds.
Tips to eat more fibre
Try and get fibre from different foods to help you have a balanced diet. You can do this by swapping some of the food you usually eat to foods with more fibre. Some simple swaps could be:
- choose a higher fibre breakfast cereal such as porridge oats, shredded wholegrain cereals or whole-wheat biscuits
- choose wholemeal or granary breads or seeded white breads
- choose brown pasta or brown rice
- add pulses, such as lentils, beans or chickpeas to stews, curries and salads
- include vegetables with every meal, and keep the skin on vegetables if possible (for example, carrots and potatoes)
- have more fruit, which can be fresh, tinned or dried fruit
- add 1 tablespoon per day of flaxseed, linseeds or chia seeds into cereals, yoghurts or soups. Remember to have an extra glass of water for every tablespoon taken.
It is very important that you have more to drink as you add more fibre into your diet. This also helps food to pass through your body and helps the poo be softer. Try and drink a glass of water with every meal and have at least 8 glasses per day. See the section on ‘I’m not drinking enough’ for tips to help this.
Does exercise help constipation?
Exercise can help constipation by helping food move through your body. In particular it can help the muscles which move poo. When you are first home from hospital after being critically ill, it can feel very tiring just beginning to move around again, so you may not be able to do extra exercise straight away. As you get stronger, you can gently start by adding in a little bit more activity, which could be walking around the house or outside, or by doing exercises in your chair. Keep slowly increasing your activity and that will help your constipation.
What else can help me if I am constipated?
Find out the best time of day when you are likely to want to go for a poo. For many people this can be 15-20 minutes after you have eaten breakfast. Try to find 10 minutes when you won’t be interrupted to try to go. However, whenever you feel like you might want to poo during the day or night, go to the toilet. It’s important not to ignore that feeling or leave it until later.
Going to the toilet is something we can often do easily, so it can feel strange to have to think about it and learn how to do it. But many things are different when recovering after a critical illness, and it can help to have tips to help you at this time. These tips can help your constipation when you are on the toilet:
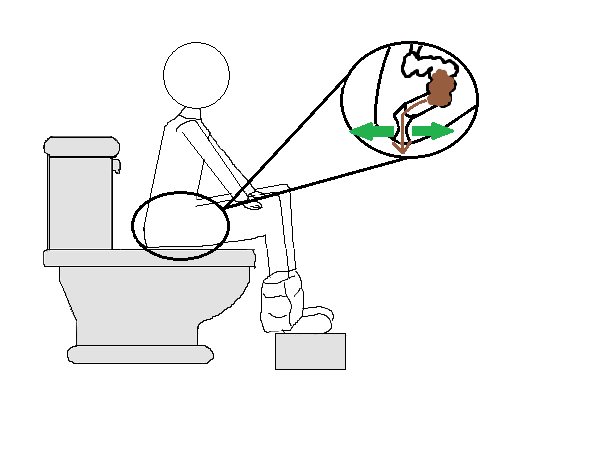
- Check your sitting position on the toilet: If possible, put your feet on something to make you sit with your knees slightly higher than your hips. Lean forward with your forearms resting on your thighs and with your back straight.
- Find out which muscles you will use: It is your waist muscles that help to push stools out of your bottom. Place your hands either side of your waist and cough. Can you feel the muscles work? When you push down you need to feel these muscles expand (move out slightly).
- Relax: Lower your shoulders. Breathe slowly and gently. Try to release all your stomach muscles and breathe so that your tummy moves in and out instead of your chest. Now push down to try to poo.
- Do not hold your breath (so do not take in a big breath first and then hold onto that breath).
- Slowly move out the muscles at your waist. You can put your hand on your waist to see if the muscles are moving. Then push from your waist downwards and backwards into your bottom, ensuring that your muscle in your back passage is relaxed and open. Do not strain.
- Relax for one second, but only slightly while you still keep some pressure at your waist without pushing with it.
- Push outwards and push downwards again. This should be repeated.
Remember: This will take time and practice. Do not spend more than 10 minutes on the toilet. Only go back to try to have another poo that day if you have the feeling that you want to poo.
What medicines may help?
If you have tried these suggestions but you are still constipated, you could try taking medicine to help you. These are called laxatives and they work by softening your poo to make it easier to go to the toilet. They are best to only take for a short time and you can stop taking them when your constipation is better, and you are going for a poo more often each week. Laxatives can be bought at a pharmacy or prescribed by your doctor.
Laxatives may be taken as a tablet by mouth (orally) or they may be a tablet which goes into your bottom. These are called suppositories. There are different types of laxatives, so speak to your doctor to find out which is best for you (and check they won’t affect other medicine you are taking). It is important that you drink enough when you are taking laxatives.
If your constipation continues, or you often need to take medicine to help it, speak to your doctor.
Summary:
If you have problems with constipation, it may help to eat different foods, drink more, look at how you go to the toilet and exercise. If you need medicine, there are several different types that your doctor will be able to advise you on. As you get stronger after your critical illness, you will be able to eat a varied healthy diet which will help good digestion and your bowels to work normally.
More information:
NHS advice on:
British Dietetic Association Food Fact Sheets on:
See ICUsteps information for more information

