Poor bowel health can be debilitating, so educating and getting people talking about their bowel habits is vital. A reported one in five people are too embarrassed to even talk to their GP about constipation, confirming that poo chat can be a taboo subject for many.1 Opening your bowels is a normal bodily function and something that each and every one of us does - so let’s chat about constipation.
What is constipation?
Constipation is a well-known term - however research found that one in five people believe that constipation is when you open your bowels less than once a day.2 The general consensus however (and included as part of the Rome IV Diagnostic Criteria for Constipation3) is that it is defined as:
- Having a poo less than three times a week
- Straining or being in pain when you have a poo
- When poo is often large and dry, hard or lumpy
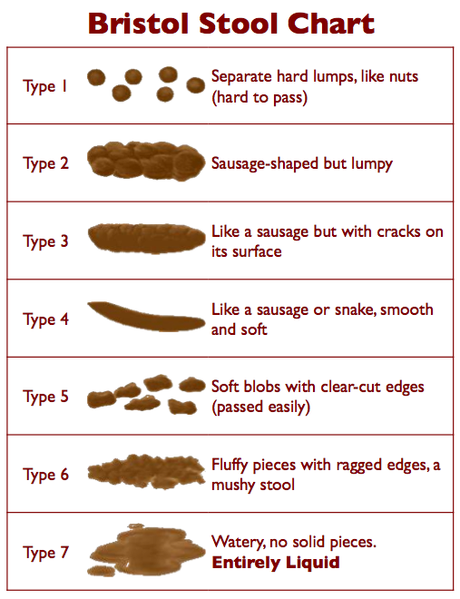
The Bristol Stool Chart is also a useful diagnostic tool.4 It is widely used across healthcare settings and can help patients communicate their stool type to their healthcare professional. Type 1 and type 2 on the Bristol Stool Chart indicate constipation.
Constipation - facts and figures
Constipation is one of the most common digestive problems affecting the UK population - so much so that it is estimated that one in seven adults and one in three children are constipated at any one time.5
Women are twice as likely to suffer from constipation; pelvic floor disorders are often a cause, as well as pregnancy, due to a change in hormones.6 It is also well recognised that the older you get, the more likely you are to be prone to constipation - approximately 26% of men and 34% of women over the age of 65 years suffer.7
In 2018-19, 76,929 people were admitted to hospital in England with constipation and a whopping £168 million was spent by NHS England treating it.1
Not only is it a huge financial burden but for those suffering with the condition, their quality of life can be hugely impacted - 40% of patients with constipation experience an anxiety disorder and 38% experience depression.8
How can you improve constipation?
Laxatives are a well-known effective treatment and like all medications, they have a time and a place but should not be seen as a ‘quick fix’. Constipation can be effectively treated for most people through diet and lifestyle changes.
Fibre
Often known as the ‘roughage’ in your diet. Fibres are plant-based carbohydrates which, unlike other nutrients, are not digested in the small intestine and therefore reach the large intestine undigested. Fibre works by bulking out stools, improving your ‘transit time’ and making stools softer and therefore easier to pass through the digestive system.
In the UK, we are recommended to eat 30g of fibre a day - however on average consumption is much less, at approximately 18g per day.9 Increasing your fibre intake is likely to help improve constipation - it is important that you make changes gradually, as increasing fibre too quickly may cause bloating or excess wind. Here are some simple suggestions for increasing your fibre intake:
- Swap to a high fibre breakfast cereal such as oats, wholewheat biscuits or bran flakes.
- Choose high fibre snacks such as a portion of fruit, a handful of nuts, oat biscuits or vegetable sticks with hummus.
- Swap to wholegrain carbohydrates such as wholewheat pasta, brown rice, wholewheat noodles and wholewheat or seeded bread.
- Add beans and pulses to your main meals such as minced meat dishes, curries or salads.
- Aim for at least one third, but try for one half, of your plate to be made up of vegetables and/or salad.
For more information and tips on how to improve your fibre intake, head to the BDA’s Fibre: Food Fact Sheet.
Fluid
Keeping yourself hydrated is vital for overall good health - and your hydration status also impacts your bowels. When you are dehydrated, the body draws out water from your stools in your large intestine to use elsewhere in the body - this can cause your stools to become dry, hard and lumpy.
The typical adult needs 1.5-2L of fluid a day, or six to eight mugs. A quick, easy way of checking your hydration status is by looking at your urine - it should be clear or a light straw colour. If you are well hydrated already, there is no evidence to suggest that increasing your fluid intake further will help prevent constipation.10
All fluids except for alcohol will count towards your fluid recommendation. However, it is important to remember other considerations for some fluids. For example, the impact of high caffeine intake from tea and coffee, particularly for pregnant women, and that fizzy drinks or fruit juices contain high amounts of sugar.
For more information and specific fluid recommendations for those in different age groups, pregnant and lactating women can be found at the BDA's Fluid (water and drinks): Food Fact Sheet.
Physical activity
Physical activity is also helpful in improving constipation. Peristalsis is the wave of muscle contractions within the gut. Peristalsis increases with physical activity and therefore can help to speed up the gut transit time and limit the amount of water that is reabsorbed from the stool in the large intestine.
The UK Government recommends that we should aim to do 150 minutes of moderate aerobic activity or 75 minutes of vigorous activity a week.11 Moderate activity includes brisk walking, dancing, water aerobics or pushing a lawnmower. Vigorous activity includes jogging, fast swimming, football, netball and gymnastics. For some people, these recommendations are not achievable but even a short walk is likely to provide some benefit.
Toilet routine
Toilet routine is just as important as other dietary and lifestyle changes and can make a real difference in improving constipation. Here are some simple tips for improving your toilet routine:12
- Aim to have a regular, unhurried routine when opening your bowels. It is important that you give yourself enough time to ensure your bowels are fully emptied.
- If you feel the urge to poo, do not ignore this. The longer your stools stay in your large intestine, the more likely they will become hard and lumpy - and therefore more difficult to pass.
- When you are sat in a 90 degree sitting position (a typical sitting position on a toilet), your bowel is ‘pinched’, making it more difficult to have a bowel movement. By sitting so that your knees are above your hips, leaning forward with your forearms on your thighs, bulging out your abdomen and straightening your spine, this will ‘straighten out’ your bowel and will make it easier for you to open your bowels.13
Can a dietitian help with constipation?
A dietitian is qualified to provide dietary and lifestyle advice for a range of clinical conditions, including constipation. They are trained to translate the most up-to-date scientific evidence into practical advice for people.
They are likely to ask about your history including past medical history and investigations, medication history, social history, anthropometrics (weight, height, weight loss, etc), any relevant clinical information such as bowel habits and symptoms, and your dietary and lifestyle habits. Based on the information provided, your dietitian will work with you as an individual to create a patient-centred plan that is specific to suit you.
If you feel it would be beneficial for you to see a dietitian, either speak to your GP and ask them to refer to your local NHS Nutrition & Dietetics department or head to the British Dietetic Association Freelance Dietitians webpage to find a dietitian who will be able to see you privately.
References
- Admissions data for ICD 10 diagnosis code K59.0 (Constipation) from April 2016 to January 2020. Accessed May 2020 from Vantage System provided by Health IQ
- YouGov research 2016
- Lacy BE, Mearin F et al (2016) 'Bowel Disorders', Gastroenterology, 150(), pp. 1393-1407
- Lewis SJ, Heaton KW (1997) Stool form scale as a useful guide to intestinal transit time. Scandinavian Journal of Gastroenterology 32: 920–4
- NHS Inform (2020) Constipation. (Accessed: 21 March 2021).
- NICE, CKS on Constipation.
- Schaefer, D. and Cheskin, L., 1998. Constipation in the Elderly. Am Fam Physician, 58(4), pp.907-914.
- Coloplast, Market Study, The impact of bowel dysfunction of patients and HCPs. 2017. Data on file [W-0196644]. (UTIs specific to NBD) Public Health England (2016)
- Government Dietary Recommendations Government recommendations for energy and nutrients for males and females aged 1 – 18 years and 19+ years
- Arnaud MJ. Mild dehydration: a risk factor of constipation? Eur J Clin Nutr. 2003 Dec;57 Suppl 2:S88-95. doi: 10.1038/sj.ejcn.1601907. PMID: 14681719.
- Department of Health & Social Care (2019) UK Chief Medical Officers' Physical Activity Guidelines
- NICE (2020) Scenario: Constipation in adults
- Continence Foundation of Australia (2020) Poor Bowel Control (Accessed: 21 March 2021).






