Wendy Frost, Advanced Dietitian in Paediatrics, reports on an audit amongst children with type 1 diabetes carried out with the aim of identifying those who are potentially more at risk of cardiovascular disease.
Children and young people with type 1 diabetes (T1D) are faced with an increased risk of developing cardiovascular disease (CVD). There is currently no consensus on managing the risk of raised cholesterol levels for this patient group.
The National Institute of Clinical Excellence (NICE) guidelines1 recommend considering statin treatment for the primary prevention of cardiovascular disease in all adults with type 1 diabetes, and offering statin treatment to adults with type 1 diabetes who are older than 40 years of age or who have had diabetes for more than 10 years.
This includes those who have established nephropathy, or other cardiovascular risk factors. These guidelines are clear for the adult population with T1D; however, there currently does not appear to be a recommendation or pathway for children and young people. The NICE guidelines for Management of Children and Young People with Diabetes 2015 do not include cholesterol screening for children with type 1 diabetes.2
The National Paediatric Diabetes Audit (NPDA, 2020-2021), however, lists annual cholesterol measurement in children over 12 as one of the seven core care processes.3
In 2017, a study by Candler et al.4 assessed the cholesterol screening of children with type 1 diabetes by sending an online survey to 280 children’s diabetes professionals. From the 87 (31%) who responded, they discovered a considerable variability in testing across centres and actions taken if levels were abnormal.
The data in this study could have been weighted to extremes, and respondents may have had strong opinions about the quality of their processes, either positive or negative. The non-respondents may have been those with no concerns regarding their practice.
The views and practices of these professionals are still a helpful indicator, despite information from all those surveyed not being reported.
Dyslipidaemia is often overlooked and inadequately treated in young people with diabetes, even though CVD remains a significant cause of mortality in adults with diabetes.5 The aetiological risk factors leading to the onset of CVD are well recognised and include hyperlipidaemia, hypertension, diabetes, obesity, smoking and lack of physical activity. They collectively represent over 90% of the CVD risks in all epidemiological studies.6
In the clinical setting, healthcare professionals may often focus on the microvascular complications of diabetes, aiming for good glycated haemoglobin (HbA1c) results and optimal ‘time in range’. Should better consideration be given to this patient group’s macrovascular complications affecting health in later life? An audit amongst children with T1D in our district general hospital was carried out with the aim of identifying those who are potentially more at risk of CVD. This was also an opportunity to explore treatments and the advice given to these individuals. Data was collected from hospital records and analysed for HbA1c, BMI percentile and lipids for children over 12 years of age in our paediatric diabetes clinic.
Audit
The study group consisted of all the over-12-year-old patients in the local hospital children and young people’s diabetes clinic. This is the starting age at which the NPDA begins to collect data, and the age that the test is first performed in the chosen clinic. This group consisted of 82 children. Of this group, there was data for cholesterol results available for 65 children. The remaining children had not yet had their test performed.
The latest recommendations suggest that screening for dyslipidaemia is recommended soon after diagnosis (when glycaemia is stabilised) in all young people with T1D from age 11 years.7
All these tests were non-fasting and formed part of the annual review process. In this trust, it is not current practice to repeat fasting lipids if they are abnormal. Studies have shown that fasting may not influence total cholesterol, LDL-C and HDL-C.8 Recent recommendations advocate re-testing if LDL-C or triglycerides (TGs) are raised.7
Smoking status and alcohol intake was discussed routinely at annual review appointments for this group. All patients in the group denied smoking or drinking alcohol regularly, and all had blood pressure readings in the ideal range.
Results
Total cholesterol
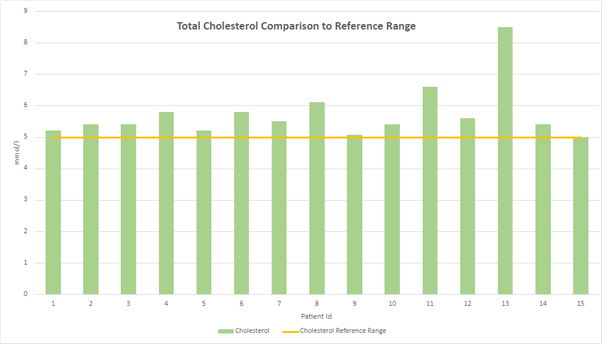
Fifteen children (23%) had cholesterol levels equal to or above the hospital reference range of 5mmol/l. None of them were known to have familial hypercholesterolaemia, although with a result over 7.5mmol/l, child number 13 has a greater risk of having this genetic disorder.9
LDL-C
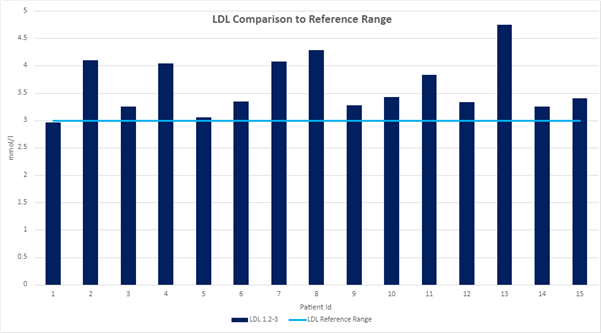
All those with raised total cholesterol levels were seen to have raised low-density lipoprotein cholesterol (LDL-C) levels, which is usual with an overall raised cholesterol.
HDL-C
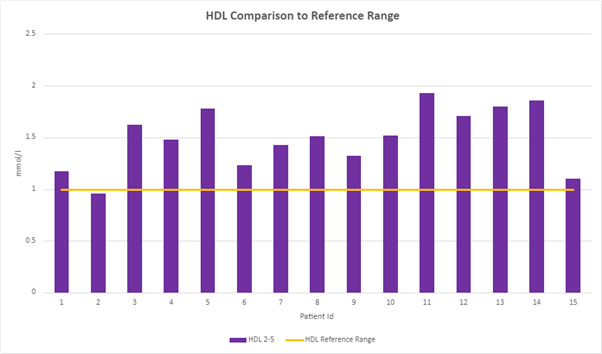
The reference range for high-density lipoprotein cholesterol (HDL-C) is 2-5mmol/l. Child number 2 was shown to have a level under 1mmol/l, a risk factor of concern. Lower values are associated with increased cardiovascular risk in T1D, which indicates less cholesterol is being transported to the liver for removal from the bloodstream.10 HDL has also been shown to have an antiatherogenic role.11
Triglycerides
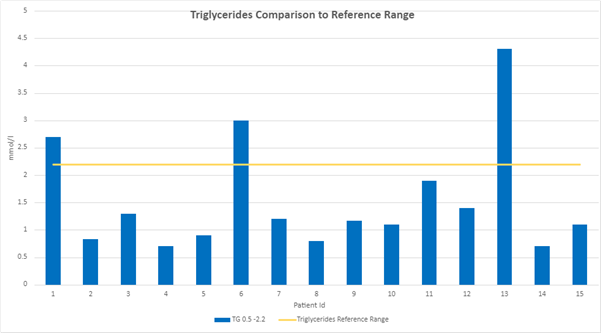
Children 1, 6 and 13 had significantly raised triglycerides (TGs). A raised TG level is a risk factor for CVD and is independent of total cholesterol.12 When TGs are elevated, lipoprotein metabolism is altered, which increases CVD risk.13
HbA1c
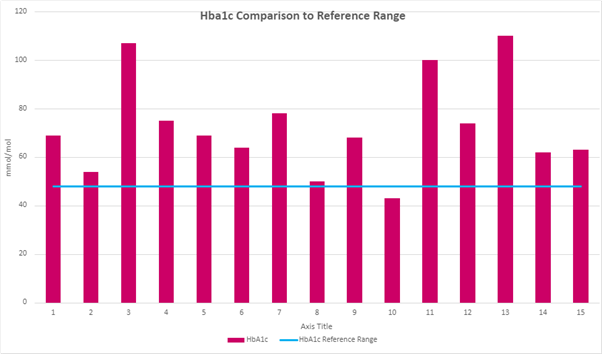
Child number 10 was the only one in the audit group who had an HbA1c below the current national recommendation of 48mmol/mol. Based on the evidence in adults with T1D, NICE recommends an overall target of 48mmol/mol, where possible, for children and young people with T1D to reduce long-term complications.2 The risk factors of high HbA1c and BMI percentiles for these 15 children were then identified.
BMI
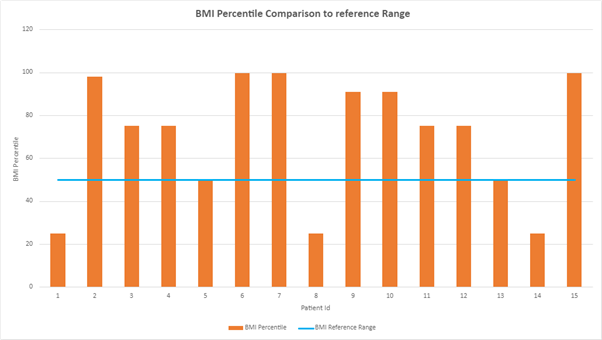
Ten of the children had BMIs over the 50th percentile. This, therefore, leaves five children who were of an ideal weight and had raised lipids. These children potentially could be consuming their recommended calorie intakes; however, they may benefit from more specific dietary interventions to improve their lipid status, for example, advice on exercise and consideration of medication.
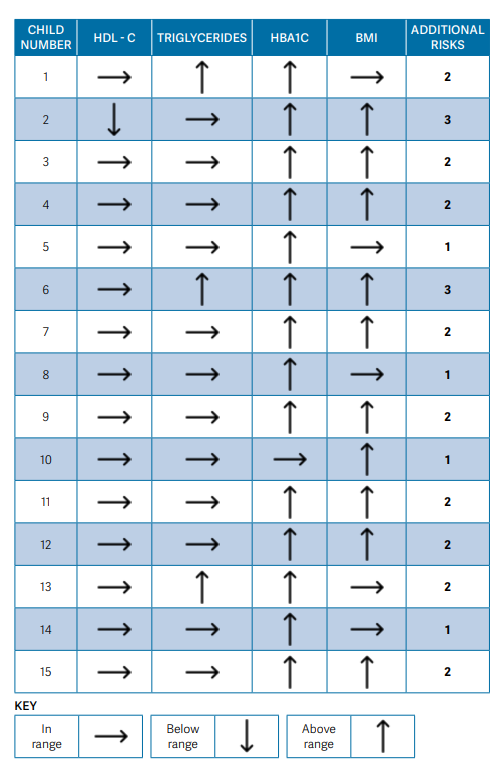
What do these results indicate?
The summary chart shows that there are other risk factors to consider in this group of children with raised cholesterol levels. It could be easy to assume that high cholesterol is merely a secondary effect of high glucose and its associated metabolic effects.14 This is not true in the findings. A commonly held belief might be that those with overweight are also those who are more likely to have raised lipids.15 However, this is not the case in this audit group. There are five children in this group with additional risk factors, including raised TGs and HbA1c levels whose BMI is considered in the ideal range. The one child with an HbA1c below the desirable range had a raised BMI. Alongside their raised lipids, this child could miss additional treatment, with good glycaemic control being the primary focus at a consultation.
Discussion
Cholesterol is a lipophilic molecule that is essential for human life. It has many roles that contribute to normally functioning cells. For example, cholesterol is a vital component of cell membranes. Cholesterol functions as a precursor molecule in the synthesis of vitamin D and steroid hormones. Cholesterol is also a constituent of bile salts used in digestion to facilitate the absorption of fat-soluble vitamins A, D, E and K. It is transported through the blood, along with triglycerides, inside lipoprotein particles. These lipoproteins can be detected in the clinical setting to estimate the amount of cholesterol in the blood.10
While cholesterol is central to many healthy cell functions, it can also harm the body if it is allowed to reach abnormal blood concentrations.10 LDL is the particle that transports cholesterol around the body and collects in the walls of blood vessels. HDL is the particle that transports cholesterol to the liver to be broken down. It is, therefore, a concern when this is too low, indicating that less cholesterol is being transported from the blood vessels to the liver for removal.
Triglycerides are the fats carried in the blood which the body uses for fuel or in excess stores as body fat. An excess in the bloodstream can occur with high blood glucose levels. High triglycerides and LDL cholesterol levels, combined with low levels of HDL cholesterol, are associated with the build-up of plaque in the arteries and a higher risk of CVD. “Consistent evidence from numerous and multiple types of clinical and genetic studies unequivocally establishes that LDL causes atherosclerotic cardiovascular disease.”16, p2460
Children with type 1 diabetes and elevated LDL cholesterol have an increased risk for cardiovascular disease, a process that can begin in childhood.17
Atherosclerosis starting in childhood and its progression is influenced by lifelong low-density lipoprotein cholesterol (LDL-C) exposure. Cardiovascular disease (CVD) represents a leading cause of death globally.18 It is a fact that many of the cardiovascular risk factors are linked, and strategies to improve glycaemia will also help with weight management and can improve lipids in many cases. Annan et al. highlighted in 2022 that hyperglycaemia, insulin deficiency and insulin resistance are associated with dyslipidaemia. Accordingly, the initial therapy should be to optimise glucose management.5
The NPDA audit 2020-21 found that 19.8% of children aged 12 years and older with T1D had a total blood cholesterol level exceeding the target of 5 mmol/l.3 This figure was 23% in the patient group studied. Most recent recommendations have suggested that a level of 4.5mmol/l would be ideal, making this risk factor of greater concern.7
The adult recommendation is to aim for a total cholesterol level under 4mmol/l.1 This would have significant implications if lower levels were targeted in the paediatric population. More intensive first-line management with diet and lifestyle modifications would require more input from healthcare professionals. An increased number of patients may feel additionally burdened by having another treatment to comply with alongside their insulin therapy. They could also potentially experience undesirable side effects from their medication. Increased usage of statins would also have huge financial ramifications for the NHS.
Current approaches
The focus of education at diagnosis is usually on glycaemic control and dose adjustment for ‘normal eating’. There are huge variations in the understanding of what a normal diet should look like and how much change is required when the diagnosis presents. To soften the blow of the diagnosis, healthcare professionals may tell families that their newly diagnosed child can continue eating their ‘normal’ diet before exploring their usual intake.
Dietary recommendations should be based on healthy eating principles suitable for all young people and families to improve diabetes outcomes and reduce cardiovascular risk.5 Consideration needs to be given when adjustments to carbohydrates are made so as not to increase dietary fats unfavourably. The Mediterranean diet of monounsaturated fats, wholegrain carbohydrates and reduced intake of red and processed meats is likely to be beneficial. Dietitians play an essential part in educating patients, their families and other health professionals.
A study by Magriplis et al.19 demonstrated that in the group of adults studied, diet and lifestyle changes related to dyslipidaemia could be achieved with continuous education, monitoring and follow-up. The key to this was the engagement of individuals. This can be a huge challenge in paediatrics, where the possible consequences of the risks are a long way off, and no immediate effects are seen. Children and young people often appear to engage better when discussing blood glucose trends, looking at continuous glucose monitor (CGM) data and achieving quick improvements that can be seen with recommended changes.
Living with type 1 diabetes carries a significant burden for the individual and family. In recent times we have had to consider the cost-of-living crisis and food insecurity more than ever before. Limited budgets can result in families buying cheaper, less nutrient-dense, high-fat, and high-sugar foods, unable to afford foods rich in unrefined grains, fresh fruit and vegetables. This can have a detrimental effect on both overall glycaemia and lipid levels. Day-to-day management of T1D involves decision-making with every mouthful of food and every activity, which poses a substantial challenge for the individual. An understanding that all children with T1D have an increased risk of CVD and identifying those who would benefit from statin treatment seems a sensible suggestion considering the lifetime of increased risk and the opportunity to improve outcomes in later life.
For many people, raised cholesterol can be improved with lifestyle changes, including increased activity, optimising BMI and following national recommendations for a healthy diet. The degree of reduction in cholesterol by diet alone, however, is often insufficient to negate the risk.20
What about drug treatment?
If the implementation of lifestyle interventions for six months does not lower cholesterol to 3.4mmol/l, with an ideal target LDL-C of 2.6mmol/l, then statins should be considered.7 When questioning colleagues across the local network, both the repeating of tests and the use of statins are not commonplace.
A study conducted by Schwab et al.21 looked at cardiovascular risk factors in patients with diabetes up to 26 years of age. They established that “despite the high prevalence of risk factors, only a small minority of patients received lipid-lowering treatment.
A combination of early identification, prevention and treatment of risk factors is necessary, considering the high incidence of future cardiovascular disease”.21, P218 Raffles et al.22 asked: “What do we do with lipid levels measured as part of the NPDA?” They concluded that pharmacological management in childhood is controversial, and the data is lacking on the benefits of lifestyle modification in this group.
Studies by Canas et al.17 concluded that atorvastatin (a commonly used lipid-lowering agent) reduced atherogenic lipoprotein sub-particles in children without worsening insulin resistance. The drug was safe and well tolerated. They recommended that long-term studies would provide better insight into the impact of these interventions in the development of CVD in children with diabetes.
A significant consideration in prescribing statins in young females is that it is contraindicated in pregnancy. Statins have a potential teratogenic risk23 as cholesterol is an integral part of cell membranes, and an agent given to reduce cholesterol could result in congenital abnormalities. Those planning a pregnancy or who cannot reliably avoid getting pregnant should not be treated with statin therapy. Oral contraceptive agents might be considered alongside starting statins.24
If prescribed appropriately and consideration is given to the individual, would statin therapy take care of one of the numerous risk factors and play a valuable part in reducing overall CVD risk? Would these children and young people benefit from the early use of statins?
Could a scoring system help to highlight those most in need of intensive advice and treatment? A pathway to follow for a consistent approach would make sense. While a national approach would be invaluable, steps have been taken at this hospital trust to address the findings from this audit to support patients most at risk.
Problems identified locally
- Family history of CVD and hyperlipidaemia is not routinely discussed at diagnosis.
- The system for keeping track of annual review blood tests and reviewing results is flawed, and a robust system for flagging raised cholesterol is not in place.
- Annual review appointments require more time for all the necessary discussions.
- No process exists for children with raised cholesterol who have not responded to diet alone after six months of receiving dietary advice.
Suggested actions
- Detailed family history to be taken at the three-month clinic review when the first HbA1c test is measured. Discussions around why this longer-term glucose level is done would tie in with those around CVD risk and avoid more overwhelming conversations at the time of diagnosis.
- The team administrator will inform the dietitian of all raised cholesterol test results so that a dietetic review can be booked, and six-monthly review blood test appointments arranged.
- A more extended appointment slot is offered for the annual review.
- Explore the possibility of using fingerpick cholesterol testing alongside HbA1c in the clinic to allow prompt and timely discussion and support engagement.
- Consider referral to a lipid specialist for advice on individual cases.
- Liaison with network lead clinicians to take this issue forward for further discussion.
An understanding and awareness from health professionals that all children with T1D have an increased risk of CVD is fundamental. Standardising the treatment pathway seems a sensible suggestion to ensure that everybody is offered optimum treatment considering the lifetime of increased risk, enabling improved outcomes in later life.
Acknowledgements
Anne Phillips and Carole Gelder, Birmingham City University Children and Young People’s Diabetes Module.
References
- National Institute for Health and Care Excellence. Cardiovascular disease: risk assessment and reduction, including lipid modification. Clinical guideline [CG181] Published: 18 July 2014 Last updated: 10 February 2023
- National Institute for Health and Care Excellence. NG18: Diabetes (type 1 and type 2) in children and young people: diagnosis and management. 2015. Last updated:29 June 2022.
- Care processes and outcomes 2020-21, RCPCH Audits National Paediatric Diabetes Audit NPDA Appendix 1 - full audit analysis.
- Candler T, Mahmoud O, Edge J, Hamilton-Shield J. Hypercholesterolaemia screening in Type 1 diabetes: a difference of opinion. Diabetic Medicine. 2017 Jul;34(7):983-6.
- Annan SF, Higgins LA, Jelleryd E, Hannon T, Rose S, Salis S, Baptista J, Chinchilla P, Marcovecchio ML. ISPAD Clinical Practice Consensus Guidelines 2022: Nutritional management in children and adolescents with diabetes. Pediatric diabetes. 2022 Dec;23(8):1297-321.
- Flora GD, Nayak MK. A brief review of cardiovascular diseases associated risk factors and current treatment regimes. Current pharmaceutical design. 2019 Oct 1;25(38):4063-84
- Bjornstad P, Dart A, Donaghue KC, Dost A, Feldman EL, Tan GS, Wadwa RP, Zabeen B, Marcovecchio ML. ISPAD Clinical Practice Consensus Guidelines 2022: Microvascular and macrovascular complications in children and adolescents with diabetes. Pediatric diabetes. 2022 Dec;23(8):1432-50.
- Schwab KO, Doerfer J, Naeke A, Rohrer T, Wiemann D, Marg W, Hofer SE, Holl RW, German/Austrian Pediatric DPV Initiative. Influence of food intake, age, gender, HbA1c, and BMI levels on plasma cholesterol in 29 979 children and adolescents with type 1 diabetes–reference data from the German diabetes documentation and quality management system (DPV). Pediatric diabetes. 2009 May;10(3):184-92.
- National Institute for Health and Care Excellence 2017a: Identification and management of familial hypercholesterolaemia (Full guideline) [National Collaborating Centre for Primary Care, 2017] and Familial hypercholesterolaemia: identification and management.
- Huff T, Boyd B, Jialal I. Physiology, cholesterol. InStatPearls [Internet] 2022 Mar 9. StatPearls Publishing.
- Kwiterovich PO Jr. The antiatherogenic role of highdensity lipoprotein cholesterol. Am J Cardiol. 1998 Nov 5;82(9A):13Q-21Q. doi: 10.1016/s0002-9149(98)00808-x. PMID: 9819099.
- Cullen P. Evidence that triglycerides are an independent coronary heart disease risk factor. The American journal of cardiology. 2000 Nov 1;86(9):943-9.
- McBride P. Triglycerides and risk for coronary artery disease. Current atherosclerosis reports. 2008 Oct;10(5):386-90.
- Parhofer KG. Interaction between glucose and lipid metabolism: more than diabetic dyslipidemia. Diabetes & metabolism journal. 2015 Oct 22;39(5):353-62.
- Feingold KR. Obesity and dyslipidemia. Endotext [Internet]. 2020 Nov 2.
- Ference, B.A., Ginsberg, H.N., Graham, I., Ray, K.K., Packard, C.J., Bruckert, E., Hegele, R.A., Krauss, R.M., Raal, F.J., Schunkert, H. and Watts, G.F., 2017. Lowdensity lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. European heart journal, 38(32), pp.2459-2472.
- Canas JA, Ross JL, Taboada MV, Sikes KM, Damaso LC, Hossain J, Caulfield MP, Gidding SS, Mauras N. A randomized, double blind, placebo-controlled pilot trial of the safety and efficacy of atorvastatin in children with elevated low-density lipoprotein cholesterol (LDL-C) and type 1 diabetes. Pediatric diabetes. 2015 Mar;16(2):79-89.
- Balder JW, Lansberg PJ, Hof MH, Wiegman A, Hutten BA, Kuivenhoven JA. Pediatric lipid reference values in the general population: the Dutch lifelines cohort study. Journal of Clinical Lipidology. 2018 Sep 1;12(5):1208-16.
- Magriplis E, Sialvera TE, Papadopoulou A, Efstathiou SP, Trautwein EA, Goumas G, Dimakopoulos I, Papavasiliou K, Koutsouri A, Zampelas A. Effectiveness and easiness of adherence to behavioural guidelines for diet and lifestyle changes for cholesterol-lowering: the Increasing Adherence of Consumers to Diet & Lifestyle Changes to Lower (LDL)Cholesterol (ACT) randomised controlled trial. Journal of Human Nutrition and Dietetics. 2019 Oct;32(5):607-18.
- Maahs DM, Dabelea D, D’Agostino Jr RB, Andrews JS, Shah AS, Crimmins N, Mayer-Davis EJ, Marcovina S, Imperatore G, Wadwa RP, Daniels SR. Glucose control predicts 2-year change in lipid profile in youth with type 1 diabetes. The Journal of pediatrics. 2013 Jan 1;162(1):101-7.
- Schwab KO, Doerfer J, Hecker W, Grulich-Henn J, Wiemann D, Kordonouri O, Beyer P, Holl RW, DPV Initiative of the German Working Group for Pediatric Diabetology. Spectrum and prevalence of atherogenic risk factors in 27,358 children, adolescents, and young adults with type 1 diabetes: cross-sectional data from the German diabetes documentation and quality management system (DPV). Diabetes care. 2006 Feb 1;29(2):218-25.
- Raffles A, Kyriakos E, Jain G, Winocour P. G572 (P) What do we do with lipid levels measured as part of the national paediatric diabetes audit?
- Karalis DG, Hill AN, Clifton S, Wild RA. The risks of statin use in pregnancy: a systematic review. Journal of clinical lipidology. 2016 Sep 1;10(5):1081-90.
- O’Gorman CS, O’Neill MB, Conwell LS. Considering statins for cholesterol-reduction in children if lifestyle and diet changes do not improve their health: a review of the risks and benefits. Vascular health and risk management. 2010 Dec 20:1-4.




